The American Gastroenterological Association is souring on the idea of probiotics.
“The public assumptions about the benefits are not well founded” notes Dr. Grace Su, professor of gastroenterology at the University of Michigan in Ann Arbor, lead author of new guidelines on probiotics just published by the AGA in the June 9 journal Gastroenterology.

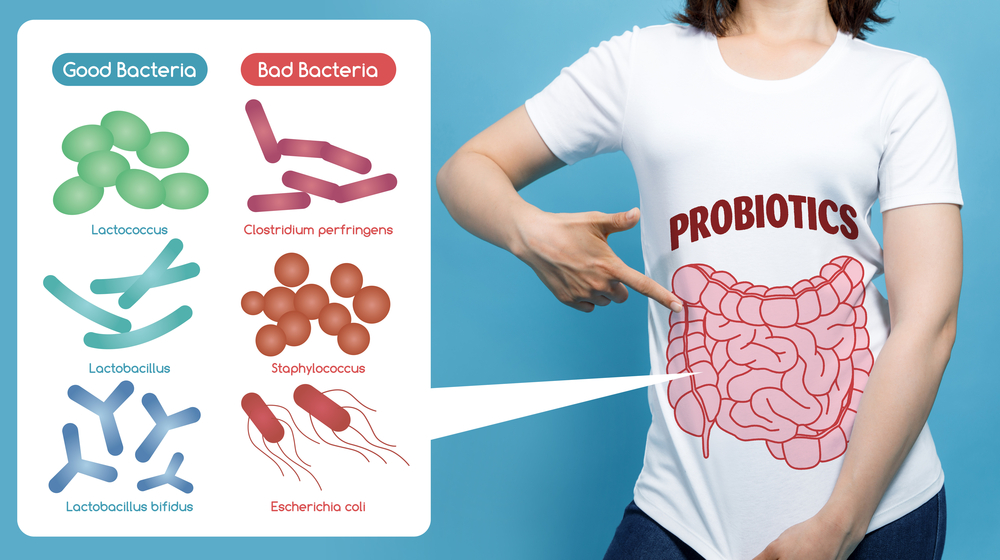
Probiotics are taken by 3.9 million Americans and are a multi-billion-dollar industry worldwide. The intention is to seed your microbiome with “good” bugs by some manufactured preparation of bacteria or yeasts, or some one of a series of ghastly seeming fermented “foodstuff” like, kombucha, kimchi, sauerkraut, or – maybe not quite so ghastly – yoghurt.
“Supplements can be costly and there isn't enough evidence to prove a benefit or confirm lack of harm” says Su and the other authors.
The conclusion is drawn from an analysis of a combination of many studies, and they do concede “conclusions drawn from meta-analyses or systematic reviews can be misleading” when trying to compare different patient populations, different reported end points and outcomes, or different strains or combinations of organisms.
They also point out that, like many natural remedies and herbal preparations, “probiotics are not considered drugs in the United States or Europe” so they are not subject to nearly same scrutiny as pharmaceutical products. And “the industry is largely unregulated, and marketing of product is often geared directly at consumers without providing direct and consistent proof of effectiveness.”
Maybe Not so Simple?
Some Arcane Exceptions
The study does recommend probiotics, but in only very limited, medical conditions - prevention of C. Difficile in the treatment of pouchitis (a complication of ulcerative colitis) and to prevent necrotizing entercolitits in preterm infants (born before 37 weeks).
It specifically recommends against their use for Crohn’s disease, ulcerative colitis, irritable bowel disease or C. Difficile infection. Or for the many people who take them because “it seems a good idea.”
The paper concludes, like almost any clinical trial you read, that “well-designed clinical trials are needed.”
Not Enough Data?
This seems another example of the “act now data later” philosophy of medical innovation
that hematologist/oncologist at the National Cancer Institute Vinayak K. Prasad MD, and Professor of Medicine at the University of Chicago, Adam S. Cifu MD MPH talk about in their great book Ending Medical Reversals – Improving Medical Outcomes, Saving Lives,